MedicVR — Iteration 1: Part 1
Research Foundations
The first iteration of MedicVR marked the beginning of an ambitious exploration into the use of Virtual Reality for medical applications. This phase focused on foundational research to understand user needs, challenges in VR environments, and the potential of immersive technology to uncover the possibilities of using Virtual Reality to bridge the gap between education and practice in medicine.
For medical students, the results underscored the need for tools that improve spatial understanding of anatomical structures and enhance their ability to interact with complex data. VR was identified as a valuable resource for bridging the gap between theoretical knowledge and practical application, ultimately supporting a more effective and engaging learning experience.
The first phase of MedicVR’s development, was primarily focused on uncovering the general challenges faced by its target audience — medical students and professionals. This exploratory phase aimed to gain a better understanding of the pain points in medical education and operational planning, particularly in the context of interacting with complex anatomical data. The research sought to answer a fundamental question: why would a Virtual Reality product be valuable for students and professors in the medical field? The interviews revealed critical insights:
These insights are supported by existing research. Cook and Triola (2009) discuss how immersive technologies like VR enhance spatial understanding and clinical decision-making, which are essential for students learning complex anatomy.1 Tang et al. (2020) further emphasize the educational benefits of augmented and virtual reality, noting their ability to improve engagement and comprehension in medical training.2 Similarly, Logishetty et al. (2019) highlight that VR tools improve precision and planning for professionals,3 while Bracq et al. (2019) underscore the cognitive and spatial benefits of VR in surgical training.4
The results for medical professionals emphasized the importance of improving training efficiency by reducing the time needed to train young professionals while maintaining high quality. Additionally, VR was seen as a tool to develop intuitive surgical workflows and enhance collaboration in medical environments.


Human Centered ERGONOMIC research
To ensure the VR application was both comfortable and accessible, the research phase incorporated principles of ergonomics and anthropometric data. The goal was to design an interface that supported prolonged use while minimizing physical strain for users.
Analysis of anthropometric data
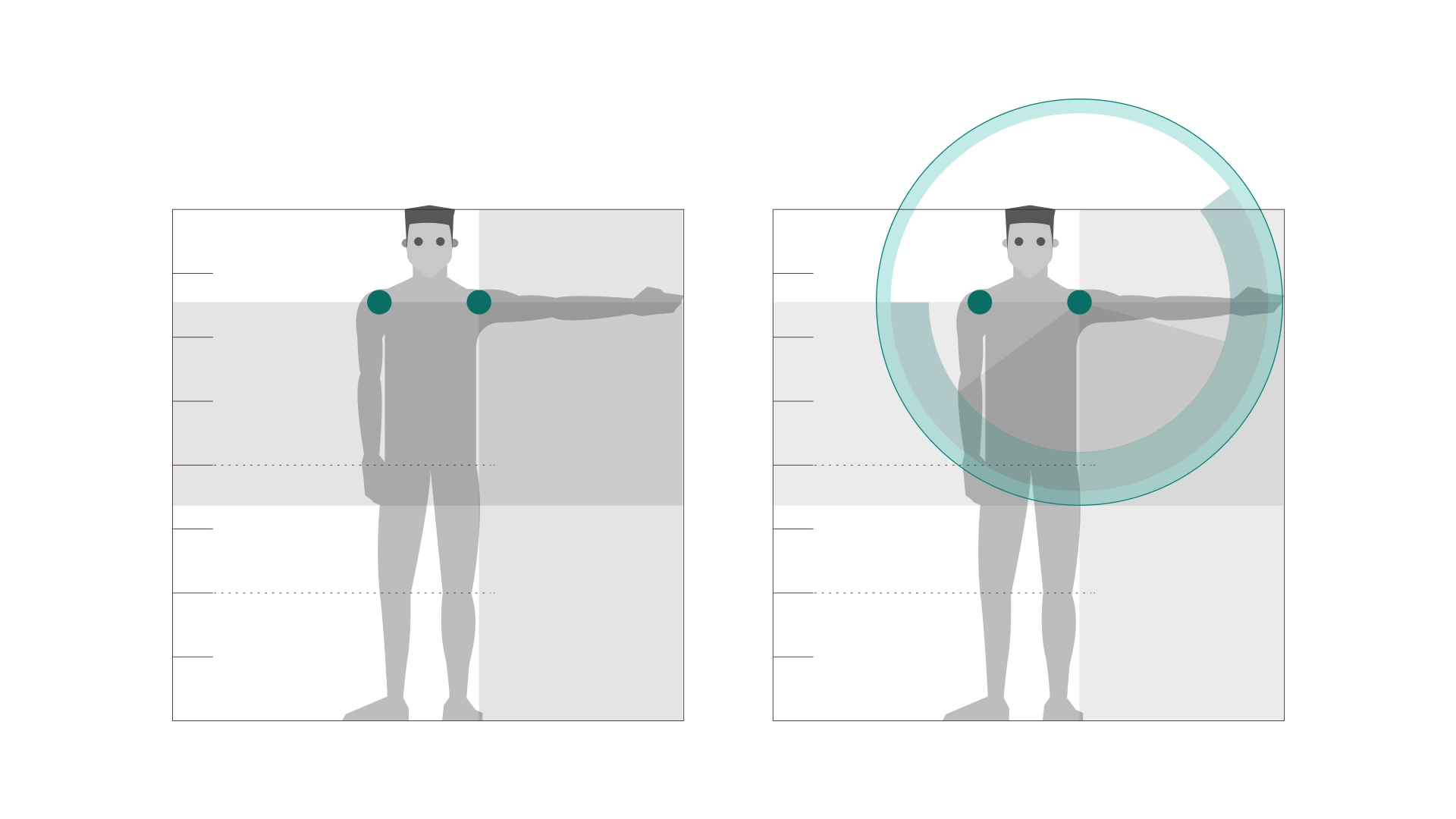
Global anthropometric data was analysed to establish ergonomic standards to ensure the interface would accommodate a diverse user base of varying sizes and physical abilities. For example, average body measurements such as arm reach and range of motion were obtained from global anthropometric data studies..5,8 These measurements informed the placement of interactive elements to help ensure they were within comfortable reach for most users.
Interaction Zones
A 3D interaction zone was determined based on the natural range of motion for the average user, reducing unnecessary strain during prolonged use. This approach was inspired by Le Corbusier's Modulor, which emphasises designing for the human scale to optimise comfort and accessibility.9 By integrating these principles, the interface ensured that all tools and menus were positioned intuitively within this zone or sight range. The design prioritized comfort to support extended sessions, particularly for medical professionals. This included:
Positioning menus and tools to minimize repetitive movements, reducing the risk of strain.6
Allowing users to alternate between standing and sitting modes, addressing fatigue and promoting flexibility.7
Ensuring visual and interactive elements were intuitively placed to maintain usability without discomfort during long periods of interaction.
Mitigating Cybersickness and Improving Immersion
Initial tests revealed significant visual distortion when curved menus were used in the VR environment. Text and icons became stretched and difficult to read, which hindered usability and user focus. To address this, the design transitioned to flat, trapezoidal menu modules. These shapes provided clarity and maximized usable space while maintaining a clean and modern aesthetic. Research by Rzayev et al. highlights that flat menu designs reduce cognitive load and improve readability in VR by minimizing distortions caused by curved surfaces.10
Cybersickness, often caused by visual disorientation and inconsistent frame rates in VR, was a key concern during development. Strategies to mitigate this included:
Menus and tools are anchored in the user’s field of view to reduce disorientation and maintain a seamless experience, minimizing unnecessary movements and keeping users focused.
The software ensures smooth visuals by maintaining consistent frame rates, reducing stuttering and cybersickness, and enabling comfortable, extended use.
Intuitive gestures, like pinching to grab, twisting to rotate, and spreading hands to zoom, mimic real-world actions, reducing the learning curve, enhancing immersion and reducing cognitive load.
Research by Brown, E., Smith, A., & Taylor, J. identifies a combination of consistent visual anchors, optimized frame rates, and intuitive interaction patterns as critical strategies to mitigate cybersickness in VR environments. 11 Additionally, Bowman et al. (2012) emphasize the importance of natural interaction models in VR, noting that gestures mimicking real-world actions significantly enhance user immersion and reduce cognitive strain.12